CRISPR ethics is an increasingly important topic as advancements in gene editing technologies reshape the landscape of medicine and biology. As we explore the potential of gene editing to combat diseases like sickle cell anemia, we are faced with profound ethical dilemmas. The power to modify genetic material raises questions about health equity and the responsibility of scientists and society to ensure fair access to these groundbreaking treatments. Bioethics, therefore, becomes essential in guiding the conversation around genetic modification and its implications for humanity’s future. As we stand on the brink of a new era in healthcare, understanding the ethical considerations surrounding CRISPR is crucial for responsible innovation.
The ethical implications of genetic engineering, particularly through techniques like CRISPR, invite a broader discussion on the morality of altering human traits and diseases. This genetic manipulation technology heralds a new age of potential cures for hereditary conditions, yet it simultaneously presents a myriad of ethical questions. Issues surrounding fairness in access to these innovations, the role of bioethics in guiding scientific progress, and the societal impact of such interventions on marginalized communities cannot be overlooked. As we weigh the benefits of solutions such as a sickle cell cure against the risks of unintended consequences, a thoughtful dialogue on health equity and responsibility in gene editing is essential. This nuanced conversation will undoubtedly shape the future of medical ethics and public health.
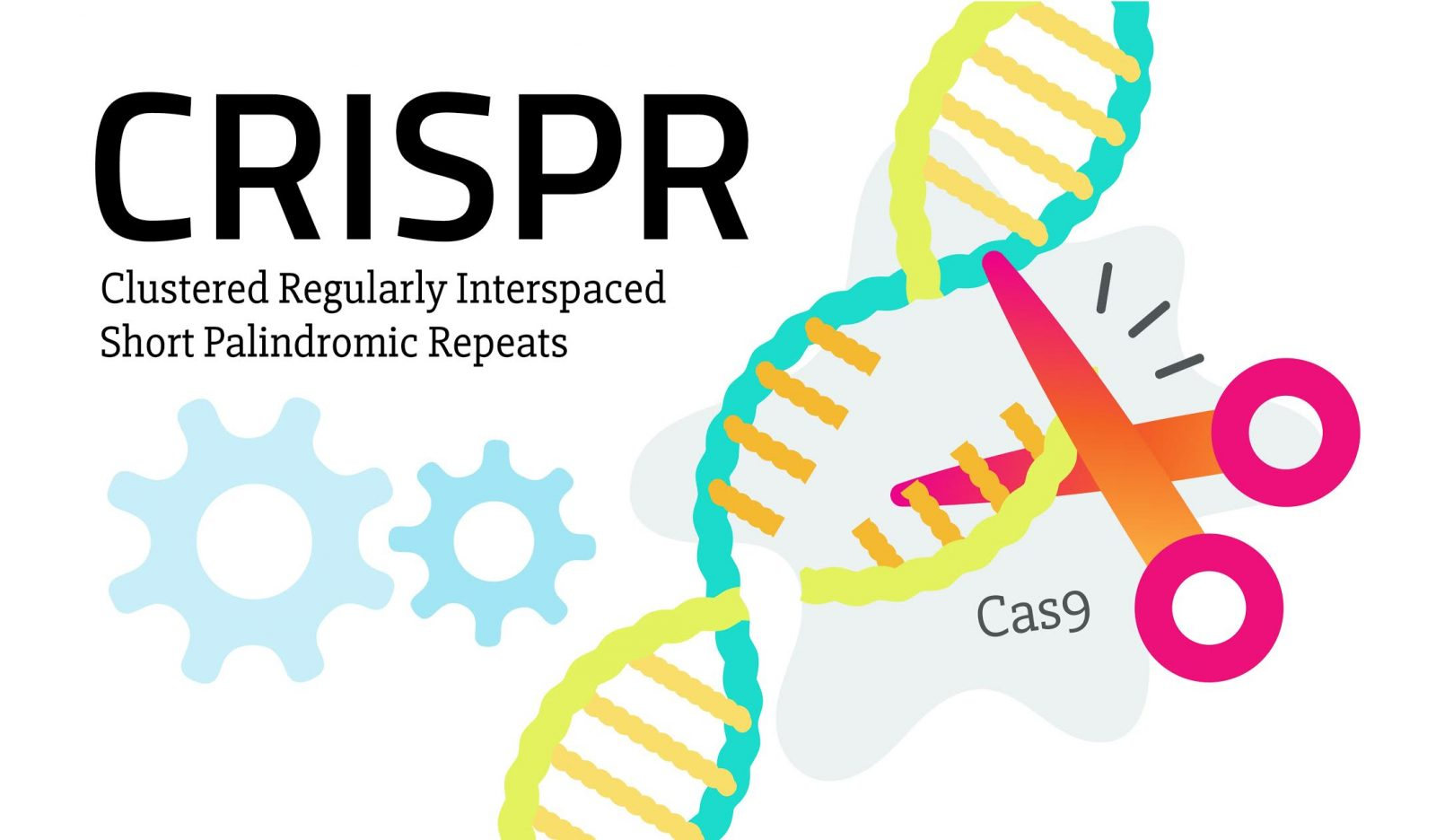
Understanding CRISPR and Its Promise for Genetic Modification
CRISPR, a revolutionary gene editing technology, carries profound implications for the future of genetic modification. It provides scientists with the ability to precisely alter DNA sequences, making once-fantastical therapies for genetic disorders like sickle cell anemia a potential reality. The capability to edit both somatic and germline cells opens up avenues not only for curing diseases but also for significant enhancements in human health and longevity. As featured in talks like “The Promise and Peril of CRISPR,” the allure of eradicating chronic illnesses is enticing, yet it raises essential considerations about how we define normalcy in human genetics.
However, the advantages of CRISPR are shadowed by ethical quandaries. The potential to use gene editing for enhancements—like increasing intelligence or physical abilities—poses questions about disparity and health equity. Will these modifications be accessible only to the wealthy, further deepening societal divides? Moreover, the implications for future generations must be thoroughly evaluated before we move forward with widespread applications of this technology, leading to debates within bioethics and health justice discussions.
Ethical Dilemmas in Gene Editing: CRISPR’s Moral Landscape
As CRISPR technology advances, so do the ethical dilemmas associated with gene editing. A core issue revolves around parental decision-making in genetic modifications; should parents be permitted to decide the traits of their children, such as the ability to hear in the case of two deaf parents? This question of agency introduces complex moral considerations, challenging societal norms about parental rights and child autonomy. The concept of genetic modification invites us to contemplate not only the potential benefits but also the societal implications of altering human traits.
Furthermore, the robustness of regulatory frameworks around CRISPR use raises significant ethical concerns. The illegal practices in countries lacking robust ethical guidelines create a fear that unregulated gene manipulation could lead to unforeseen consequences, including the proliferation of designer babies. Experts like Baer emphasize the necessity of a careful approach, advocating for transparent discussions surrounding innovation in genetics and its impact on diverse populations, particularly vulnerable communities that could face inequitable access to these groundbreaking therapies.
Health Equity in the Age of CRISPR: A Call for Justice
The application of CRISPR technology in curing diseases such as sickle cell anemia presents a unique challenge regarding health equity. As discussed in Harvard’s insights, the hefty price tag of approximately $2.2 million for gene editing poses a serious question: who can afford these transformative treatments? The disparity in access to advanced medical interventions can exacerbate existing health disparities among different socioeconomic groups. Thus, addressing health equity in biotechnology must be a priority as we navigate the implications of CRISPR.
Moreover, the conversation around equitable access must extend beyond mere affordability; it also includes considerations of who gets to determine the allocation of these resources. Policymakers and bioethicists must collaborate to develop frameworks ensuring that gene editing advancements do not favor those already in privileged positions but instead strive for inclusivity and equal opportunity for all individuals, regardless of their background. Only through an equitable approach can we harness CRISPR’s potential while remaining true to the ethical responsibility of promoting health justice for all.
The Future of CRISPR: Innovation and Oversight
As CRISPR technology paves the way for unprecedented medical innovations, it also necessitates stringent oversight to mitigate the risks associated with gene editing. The talk by Neal Baer highlighted the alarming potential of unregulated research, particularly in countries where cloning and germline modifications might occur without adequate legal constraints. The lack of global consensus on ethical guidelines for gene editing presents a formidable challenge, requiring collaborative international efforts to ensure responsible use of this powerful technology.
Innovation must be accompanied by robust ethical frameworks and regulatory oversight that prioritize safety while balancing scientific advancement. Regular assessments and transparent discussions about the implications of CRISPR usage will be critical in shaping policies that prevent misuse and unintentional harm. Only by establishing accountability measures can we foster an environment where gene editing serves humanity’s best interests, rather than compromising ethical standards in the pursuit of scientific exploration.
CRISPR’s Role in Curing Sickle Cell: Hope with Caution
The potential of CRISPR in curing sickle cell disease is a beacon of hope for many suffering from this debilitating condition. By directly modifying the genes that cause sickle cell, researchers are awakening the prospect of not just alleviating symptoms but entirely eradicating the disease. As illustrated in Neal Baer’s discussions, such advancements could radically transform the lives of thousands, sparking enthusiasm for further research and investment in gene editing technologies.
However, the road to implementation is fraught with ethical questions and practical considerations. The high cost of these treatments raises concerns about their accessibility to lower-income populations, exacerbating issues of health equity. As the global community navigates the complex landscape of gene editing, it is essential to balance the excitement over potential cures with a careful examination of the wider societal implications and ethical considerations surrounding these groundbreaking treatments.
Bioethical Considerations in Genetic Modification
Bioethics enters a critical role in discussions surrounding genetic modification and the use of technologies like CRISPR. As we stand on the brink of potentially altering human genetics, it is imperative to engage in conversations that question the morality of such actions. The implications extend beyond individual cases to encompass the fabric of society, asking us to consider what it means to be human and whether we have the right to alter our natural genetic makeup.
Further, engaging bioethics in the realm of genetic modification encourages a holistic approach that integrates perspectives from various disciplines. Involving ethicists, scientists, policymakers, and the public in dialogue ensures that a diverse range of viewpoints is considered, fostering a comprehensive understanding of the unfolding consequences associated with gene editing. This kind of interdisciplinary engagement is necessary for developing policies that reflect our collective values while guiding responsible innovation.
The Intersection of Gene Editing and Health Policies
The advent of gene editing technologies like CRISPR necessitates a reexamination of current health policies. As we unlock new capabilities for altering human genetics, there emerges a vital need to adapt existing regulatory frameworks to accommodate the complexities introduced by these innovations. This alignment will facilitate responsible research while safeguarding public health interests and ensuring ethical standards are broadly adhered to.
Moreover, formulating responsive health policies requires input from multiple stakeholders, including researchers, healthcare practitioners, and communities affected by genetic diseases. Collaborative efforts among these groups will be essential in crafting health policies that protect individuals’ rights while fostering an atmosphere of scientific inquiry and advancement. By proactively engaging with these issues, we can develop an ethical pathway for integrating gene editing into mainstream medical practices.
Public Perception of CRISPR: Navigating Acceptance and Fear
Understanding public perception of CRISPR technology is paramount for its successful integration into health care. Many individuals remain wary of the unknown repercussions associated with genetic modification. The emotional weight of altering fundamental aspects of human biology evokes fear and resistance, underscoring the importance of transparent communication about the potential advantages and inherent risks of gene editing. Educational efforts must aim to demystify CRISPR and cultivate informed discourse that empowers individuals to engage directly with scientific advancements.
Involving community voices in this conversation can play a significant role in bridging gaps between scientific communities and the public. By creating platforms for dialogue, scientists can better understand local concerns about gene editing while simultaneously addressing misconceptions. This two-way street fosters a sense of trust and cooperation, ultimately paving the way for broader acceptance of CRISPR as a tool for improving health outcomes.
Gene Editing Innovations: A Global Perspective
The realm of gene editing, particularly with advancements like CRISPR, requires a robust global perspective to ensure responsible usage and equitable access to its benefits. Different countries approach bioethics and health regulations diversely, resulting in a patchwork of standards that can lead to imbalances in how these technologies are utilized. Developing a cohesive international framework will be essential in managing gene editing practices and ensuring that innovations do not exacerbate existing inequalities.
Furthermore, international collaborations can provide insight into best practices for gene editing applications, incorporating lessons learned from varied ethical frameworks and regulatory environments. By working together, nations can facilitate a more equitable distribution of resources and information surrounding CRISPR technology, leading to global advancements in health equity and innovation. Such partnerships can also promote transparency and trust among participating stakeholders, enriching the dialogue around the future of genetic modification.
Frequently Asked Questions
What are the ethical implications of gene editing using CRISPR technology?
The ethical implications of gene editing using CRISPR technology are significant and multifaceted. This technology allows for precise modifications in genes, raising concerns about the morality of altering human traits and the potential consequences of such changes. Issues such as parental autonomy in selecting traits for their children, the disparity in access to these treatments, and the long-term effects on human genetics and biodiversity are central to the CRISPR ethics debate.
How does CRISPR technology relate to health equity in gene editing for diseases like sickle cell?
CRISPR technology offers potential cures for diseases such as sickle cell anemia, but raises vital health equity questions. The exorbitant cost of some gene-editing therapies can limit access, creating a divide between those who can afford treatment and those who cannot. This disparity highlights the need for ethical frameworks that ensure fair distribution of gene editing benefits, aiming to avoid further health inequalities.
Should CRISPR be used for genetic modification of conditions like Down syndrome?
The use of CRISPR for genetic modification of conditions like Down syndrome is a contentious ethical topic. While gene editing could potentially eliminate certain disabilities, it also prompts questions about societal values and acceptance of human diversity. The decision-making power regarding such interventions must be approached with caution and involve comprehensive ethical considerations to avoid undermining the dignity of individuals with disabilities.
What role do bioethics play in the application of CRISPR technology in medicine?
Bioethics plays a crucial role in the application of CRISPR technology in medicine by guiding the moral frameworks surrounding gene editing. It addresses important concerns such as consent, the impact on future generations, and the prioritization of health-related interventions. Bioethics ensures that advancements in CRISPR are aligned with societal values and do not exploit vulnerable populations or exacerbate health disparities.
What are the potential unintended consequences of gene editing with CRISPR?
Potential unintended consequences of gene editing with CRISPR include off-target effects, where unintended sections of DNA may be altered, leading to unforeseen health issues. Additionally, manipulating single genes can disrupt complex biological interactions, which might result in new genetic conditions or health challenges. Understanding these risks is crucial for ethical vetting before widespread implementation of CRISPR technology.
How does genetic modification through CRISPR affect the concept of ‘human variation’?
Genetic modification through CRISPR challenges the concept of ‘human variation’ by introducing a paradigm where certain traits may be deemed undesirable and subject to elimination. This raises profound ethical concerns about the idea of normalcy and the value of diversity. Many argue that variations like deafness or other differences should be embraced rather than altered, highlighting the need for a broader understanding of human identity beyond genetic definitions.
Who is responsible for overseeing CRISPR practices globally?
The oversight of CRISPR practices globally is complex, as there is currently no unified regulatory body governing gene editing across all countries. Variations in laws and ethical standards create challenges, leading to concerns about rogue scientists operating in less regulated environments. Vigilant and comprehensive international cooperation is critical to ensure that CRISPR technology is used responsibly and ethically worldwide.
| Key Points |
|---|
| CRISPR is a gene-editing technology that enables significant advancements in treating genetic diseases like sickle cell anemia. |
| The ethical dilemma centers around whether we should alter human traits and the implications of doing so. |
| Gene editing could result in unjust practices, as expensive treatments may not be available to all, raising questions about health equity. |
| There are concerns about parental control over genetic modifications for non-life-threatening conditions. |
| The potential for unintended consequences arises from gene editing, as genes have complex interactions. |
| Global oversight for CRISPR research is problematic, raising concerns about ethical standards in different countries. |
Summary
CRISPR ethics is a vital concern in today’s medical landscape as we grapple with the implications of gene editing technologies. While CRISPR presents the potential to cure serious diseases such as sickle cell anemia, it also introduces troubling ethical dilemmas regarding the modification of human traits, equity in healthcare access, and the decision-making power of parents regarding their children’s genetic futures. The call for strong ethical oversight and consideration of health justice is paramount as we navigate these revolutionary scientific advancements.