Pediatric Cancer AI Prediction represents a groundbreaking advancement in the battle against childhood brain tumors, particularly gliomas. Recent research highlights the power of artificial intelligence in pediatric oncology, showcasing its ability to predict cancer relapse with remarkable accuracy compared to traditional methods. By leveraging advanced machine learning techniques, including temporal learning models, this AI tool meticulously analyzes multiple brain scans over time, offering invaluable insights into pediatric glioma recurrence risk. This innovative approach not only alleviates the stress associated with frequent follow-ups but also enhances the treatment strategies for young patients. As we progress further into the realm of AI in healthcare, the implications of these findings could revolutionize how we manage cancer relapse predictions in pediatric populations.
The emergence of artificial intelligence in the realm of pediatric cancer prediction marks a significant milestone in healthcare innovation. Utilizing sophisticated algorithms and machine learning, researchers are now able to forecast outcomes in young cancer patients with much greater precision. These predictive models, especially in the context of pediatric glioma recurrence, hinge on continuous monitoring through successive medical imaging. Such technology promises to refine how healthcare providers assess cancer relapse risks, making follow-up protocols more efficient and less invasive. With promising results emerging from recent studies, the path forward looks bright for integrating AI tools into pediatric oncology practices.
Advancements in AI for Pediatric Oncology
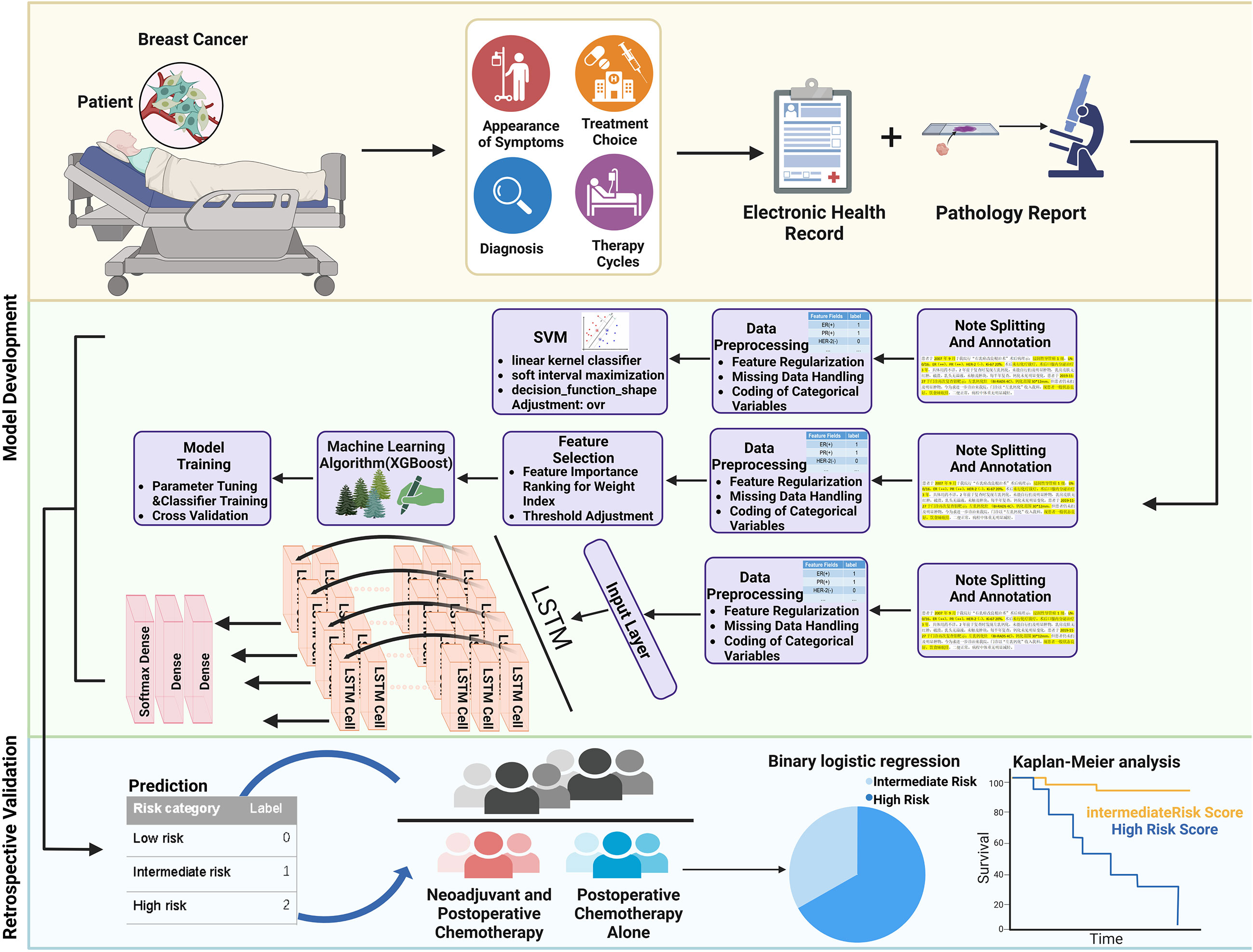
Recent advancements in artificial intelligence (AI) are transforming the landscape of pediatric oncology by providing enhanced predictive analytics for cancer relapse. The integration of AI tools has allowed researchers to delve deeper into the diagnosis and management of pediatric cancers, particularly in developing machine learning models that forecast the risk of recurrence. By analyzing vast datasets and numerous brain scans over time, these tools facilitate a more personalized approach to treatment, optimizing outcomes for young patients.
A notable application of AI in pediatric oncology is the use of algorithms to process multiple imaging scans, which helps in identifying subtle changes indicative of tumor relapse. Such methods diverge from traditional techniques, which often rely on isolated images, enhancing the reliability of cancer relapse predictions. This evolution in leveraging data analytics underscores the promising future of machine learning in healthcare, as it not only streamlines patient assessment but also enriches clinical decision-making.
Understanding Pediatric Glioma Recurrence
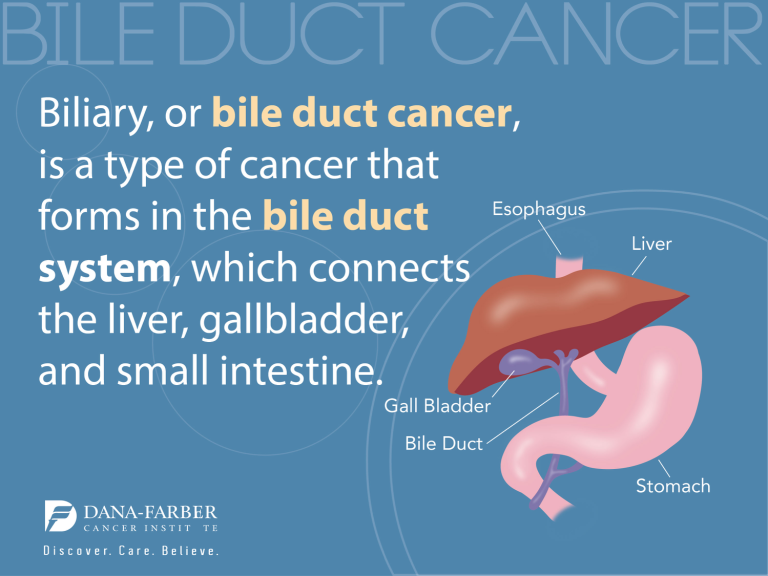
Pediatric gliomas represent a significant challenge within the sphere of childhood cancers due to their complex nature and varying treatment outcomes. These brain tumors, although often manageable through surgical intervention, pose a substantial risk of recurrence that can greatly affect the quality of life for affected children. Understanding the patterns of these recurrences is crucial for oncologists, as it informs ongoing treatment strategies and follow-up care.
Factors contributing to glioma recurrence can vary widely, from the tumor’s molecular characteristics to the initial treatment approach. Traditional methods of predicting pediatric glioma recurrence have proven inadequate, often leading to unnecessary stress for patients and families due to frequent imaging testing. However, with the incorporation of AI tools like temporal learning models, clinicians are now able to make more informed predictions that can potentially minimize the frequency of MRIs and tailor follow-up care to individual risk profiles.
The Role of Temporal Learning Models in Predicting Cancer Relapses
Temporal learning models represent a revolutionary advancement in the predictive analytics of pediatric cancer treatment, especially in analyzing sequential imaging data post-surgery. Unlike conventional AI models that assess single scans, these cutting-edge approaches assimilate information from a series of brain scans over time. This methodology allows for a deeper understanding of tumor behavior and recurrence risk, enabling healthcare providers to make data-driven decisions with greater confidence.
By organizing a patient’s MR scans chronologically, temporal learning models can detect minute variations that may signal early signs of relapse, offering a significant enhancement over traditional prediction methods. The accuracy rates observed in recent studies highlight the capacity of these models to accurately forecast relapses, bridging a critical gap in pediatric care and emphasizing the value of continuous and longitudinal patient monitoring.
AI in Pediatric Cancer Risk Management
The implementation of AI in pediatric cancer risk management is reshaping treatment protocols and follow-up strategies for children diagnosed with malignancies. By employing advanced machine learning techniques, healthcare professionals can identify high-risk patients early, allowing for tailored interventions that could mitigate the likelihood of cancer relapse. These predictive analytics not only prioritize patient safety but also empower families with actionable insights regarding their child’s treatment.
Moreover, the potential to reduce the frequency of follow-up MRIs for low-risk patients demonstrates how AI can streamline healthcare delivery, freeing up resources and minimizing the emotional burden on children and their families. As AI continues to evolve within the realm of pediatric oncology, its role in risk management will likely become increasingly crucial, providing tools that support better clinical outcomes and improved patient experiences.
Machine Learning in Healthcare: A Paradigm Shift
Machine learning is ushering in a paradigm shift in healthcare, particularly within the domain of oncology where predictive modeling and tailored treatments are becoming more prevalent. By leveraging large datasets and employing sophisticated algorithms, medical professionals can uncover hidden patterns in patient data that would otherwise remain obscured. This capability is particularly beneficial in pediatrics, where understanding disease progression can lead to more effective treatment plans.
The use of machine learning in predicting cancer relapse demonstrates its practical application in real-world settings. Many healthcare systems are beginning to adopt these tools to enhance diagnostic precision and treatment efficacy. By continuously refining algorithms based on new data and outcomes, machine learning holds the promise of delivering progressively better predictions and treatments, ultimately benefiting younger patients grappling with cancer.
Clinical Trials and AI in Pediatric Cancer Prediction
As AI tools continue to demonstrate their value in predicting pediatric cancer outcomes, the need for clinical trials to validate these methodologies becomes increasingly apparent. Ongoing research aims to bridge the gap between AI-driven predictions and clinical practice, ensuring that these innovations can be integrated effectively into patient care protocols. The goal is to establish concrete evidence that reinforces the reliability and effectiveness of AI in managing pediatric cancers, specifically in improving relapse risk assessments.
Engaging in clinical trials involving AI predictions will also facilitate greater understanding of patient responses to treatments and improve the development of personalized therapy regimens. The commitment to rigorous testing underscores the healthcare community’s resolve to adopt evidence-based practices that prioritize patient welfare while also advancing technological integration in oncology care.
Ethical Considerations in AI Deployment
While the promise of AI technology in predicting cancer outcomes is immense, it also raises significant ethical considerations. As healthcare professionals increasingly rely on machine learning models for critical decisions regarding pediatric cancer treatment, issues surrounding data privacy, algorithmic bias, and informed consent become pivotal. Ensuring that AI tools align with ethical standards is essential for maintaining trust between patients, families, and healthcare providers.
Moreover, the question of accountability in decisions driven by AI systems warrants careful examination. Clear guidelines must be established to delineate responsibilities among clinicians and technology developers, particularly in cases where algorithm predictions directly influence patient outcomes. Addressing these ethical dimensions is not only critical for the safe implementation of AI but also vital for the broader acceptance of these innovations in healthcare.
Future Directions in Pediatric Oncology with AI
The future of pediatric oncology is poised for transformation as AI technologies continue to evolve and integrate into clinical practice. Emerging research indicates that these tools could lead to groundbreaking advancements in early detection, timely interventions, and the overall management of pediatric cancers. With ongoing developments in machine learning and data analytics, the potential for enhanced predictive capabilities and personalized treatment plans becomes increasingly tangible.
Looking ahead, collaboration between technological innovators and healthcare providers will be crucial in refining AI models for pediatric oncology. This partnership is essential in harnessing the full potential of AI, ensuring that the tools developed are not only technically proficient but also clinically relevant. As researchers continue to explore and validate novel applications of AI in pediatric cancer care, the journey toward improved outcomes for young patients is gaining momentum.
Integration of AI Tools in Clinical Settings
As the capabilities of AI tools in predicting pediatric cancer recurrence become more evident, the integration of these technologies into clinical settings is paramount. Healthcare institutions are starting to recognize the value of utilizing AI-driven insights to inform clinical decision-making processes and enhance patient care pathways. This shift towards evidence-based AI applications aims to create a seamless blend of technology and human expertise in oncology settings.
The implementation of AI systems in hospital settings not only empowers clinical teams with advanced analytics but also fosters a culture of continuous improvement in patient management. By equipping oncologists with data-backed predictive tools, hospitals can prioritize proactive measures, improving the quality of life for pediatric patients facing cancer. A smooth integration of AI will require ongoing training and adaptations to existing workflows, yet the potential benefits for patient outcomes underscore its necessity.
Frequently Asked Questions
How does Pediatric Cancer AI Prediction improve glioma recurrence forecasts?
Pediatric Cancer AI Prediction employs advanced machine learning techniques, specifically a temporal learning model, to analyze sequences of brain scans over time. This approach allows clinicians to understand subtle changes and accurately predict the risk of glioma recurrence, outperforming traditional methods that rely on single images.
What role does machine learning play in pediatric oncology?
Machine learning in healthcare, particularly in pediatric oncology, enhances diagnosis and treatment predictions. By analyzing vast amounts of imaging data, like in Pediatric Cancer AI Prediction, machine learning algorithms can identify patterns and risks associated with cancer relapse, leading to more personalized and effective care.
What are the benefits of using AI for cancer relapse predictions in children?
Using AI for cancer relapse predictions in children offers several benefits, including improved accuracy in forecasting risks of recurrence, reducing unnecessary follow-up procedures, and providing tailored treatment plans based on the individual’s unique recovery patterns observed through sequential MR scans.
How does temporal learning contribute to cancer predictions in pediatric patients?
Temporal learning models analyze multiple brain scans taken over time, which helps in detecting changes that single-image analysis might miss. This innovative approach in Pediatric Cancer AI Prediction allows better assessment of glioma recurrence risk, enhancing the likelihood of timely and appropriate interventions.
Are the results from the Pediatric Cancer AI Prediction study reliable?
Yes, the results from the Pediatric Cancer AI Prediction study show a significant improvement in predicting glioma recurrence risk, achieving an accuracy rate of 75-89%. However, further validation in clinical settings is necessary before fully implementing these findings in practice.
What insights did the recent study on pediatric glioma and AI provide?
The study highlighted that integrating AI with temporal learning in analyzing patient MR scans can lead to accurate predictions of glioma recurrence, a crucial advance in pediatric oncology that aims to improve patient outcomes and streamline follow-up care.
How might AI tools revolutionize care for pediatric cancer patients?
AI tools, such as those used in Pediatric Cancer AI Prediction, could revolutionize care by enabling risk stratification among pediatric cancer patients, optimizing treatment plans, reducing unnecessary imaging, and ultimately enhancing quality of life for children and their families during recovery.
| Key Point | Description |
|---|---|
| AI Prediction Accuracy | The AI tool predicts the risk of relapse in pediatric cancer patients with an accuracy of 75-89%, significantly better than traditional methods which have a 50% accuracy. |
| Temporal Learning Methodology | This approach uses multiple brain scans over time to detect subtle changes, thereby improving prediction accuracy. |
| Impact on Pediatric Gliomas | Many pediatric gliomas can be treated successfully, but the risk of relapse remains a significant concern that this AI tool aims to address. |
| Future Steps | Further validation studies and clinical trials are planned to assess clinical implementation and improve patient care strategies. |
Summary
Pediatric Cancer AI Prediction is set to revolutionize how we approach cancer care for children, particularly for those at risk of glioma relapse. The innovative AI tool discussed in the recent study highlights the importance of predictive analytics in enhancing treatment outcomes and patient quality of life. By utilizing advanced techniques like temporal learning, the tool not only improves the accuracy of relapse predictions but also provides a framework for future AI applications in pediatric oncology. With ongoing research and clinical trials, we have the potential to significantly change management strategies and improve the overall care for young cancer patients.