Maternal mortality remains a critical issue in the U.S., ranking alarmingly high among high-income countries, with a growing rate of pregnancy-related deaths. Recent studies reveal that over 80 percent of these fatalities are preventable, emphasizing the urgent need for improved prenatal care and postpartum support. The persistent healthcare disparities contribute significantly to the rise, with certain racial and ethnic groups facing disproportionately high risks during and after pregnancy. For instance, American Indian and Alaska Native women experience nearly four times the mortality rate of their white counterparts, highlighting the need for systemic changes in maternal health policies. Addressing the root causes of maternal mortality and disparities is essential for safeguarding mothers and ensuring healthy futures for their children.
The term “maternal mortality” encompasses the tragic phenomenon of deaths related to pregnancy and childbirth, impacting women across various demographics. In recent analyses, the alarming statistics surrounding pregnancy-related fatalities, also referred to as pregnancy-associated deaths, have drawn attention to the shortcomings in maternal healthcare systems. With a pronounced focus on enhancing maternal health services, improving prenatal and postpartum care is crucial to combat this alarming trend. Significant attention is needed to rectify U.S. healthcare disparities that disproportionately affect vulnerable populations and contribute to increased risks during the perinatal period. In recognizing the importance of comprehensive care, we open avenues to mitigate these preventable losses; a critical step toward equitable health outcomes.
Understanding Maternal Mortality Rates in the U.S.
Maternal mortality rates in the United States remain a concerning public health crisis, with recent studies indicating a continued rise in pregnancy-related deaths compared to other high-income countries. This trend is alarming, especially given that over 80% of these deaths are preventable with access to proper care and resources. The U.S. healthcare system is marked by significant disparities, primarily influenced by factors such as race, socio-economic status, and geographical location. When analyzing maternal mortality rates, these disparities become glaringly apparent, with marginalized communities facing disproportionately higher rates of pregnancy-related deaths.
The statistics surrounding maternal mortality are staggering, highlighting a disturbing trend where American Indian and Alaska Native women experience mortality rates nearly four times that of their white counterparts. This racial disparity underscores how systemic inequities within U.S. healthcare contribute to worse outcomes for women of color. Addressing these disparities requires a multifaceted approach that not only seeks to improve healthcare access but also confronts the deep-seated biases that exist within medical institutions.
Frequently Asked Questions
What are the main causes of maternal mortality in the U.S.?
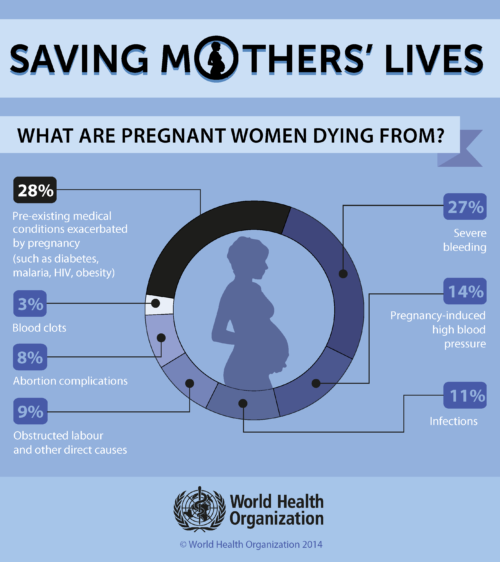
Maternal mortality in the U.S. is primarily caused by cardiovascular diseases, which now account for over 20% of pregnancy-related deaths. Other critical factors include complications from hemorrhage, infections, and underlying chronic conditions like hypertension and diabetes. Addressing these issues through improved prenatal care and postpartum support is essential to reduce maternal deaths.
How do U.S. maternal mortality rates compare to other high-income countries?
The U.S. has the highest maternal mortality rate among high-income countries, with over 80% of pregnancy-related deaths deemed preventable. Factors contributing to this disparity include a fragmented healthcare system, inequitable access to care, and significant racial and ethnic disparities in maternal health outcomes.
What role do healthcare disparities play in maternal mortality?
Healthcare disparities significantly impact maternal mortality rates, particularly among racial and ethnic minorities. For example, American Indian and Alaska Native women experience the highest maternal mortality rates, nearly four times that of white women. Addressing these disparities through equitable access to quality maternal health care is crucial for improving outcomes.
Why is postpartum care important for preventing maternal mortality?
Postpartum care is vital in preventing maternal mortality, as nearly a third of pregnancy-related deaths occur between 42 days and one year after childbirth. Improved postpartum support and follow-up care can help identify and manage health complications, ultimately reducing the risk of late maternal deaths.
What measures can be taken to reduce maternal mortality rates in the U.S.?
To reduce maternal mortality rates, comprehensive strategies must be implemented, including enhancing access to quality prenatal care, extending postpartum support, and addressing systemic disparities within the healthcare system. Investing in public health infrastructure and innovative care models can significantly improve maternal health outcomes.
How has the COVID-19 pandemic impacted maternal mortality rates?
The onset of the COVID-19 pandemic in 2020 correlated with a sharp increase in maternal mortality rates in the U.S. By 2022, these rates remained higher than pre-pandemic levels. The pandemic exacerbated existing healthcare disparities and limitations in maternal health services, underscoring the need for robust healthcare reforms.
What is the significance of ‘late maternal deaths’ in maternal mortality statistics?
‘Late maternal deaths’ refer to deaths occurring between 42 days and one year postpartum and make up a significant portion of pregnancy-related mortality. Recognizing these deaths as part of maternal health statistics highlights the importance of ongoing healthcare support beyond the traditional six-week postpartum check-up.
Can maternal mortality be reduced through policy changes?
Yes, policy changes aimed at improving maternal health access, particularly in underserved regions, can significantly contribute to reducing maternal mortality. States can learn from successful models, like those in California, which demonstrate the effectiveness of comprehensive policies in improving health outcomes.
How does chronic health condition prevalence affect maternal mortality?
The rising prevalence of chronic health conditions, such as hypertension and diabetes, among individuals of reproductive age is linked to higher maternal mortality rates. As these conditions occur more frequently in younger populations, they pose significant risks during pregnancy, necessitating focused public health interventions.
What is the relationship between access to prenatal care and maternal mortality?
Access to quality prenatal care is crucial in reducing maternal mortality. Comprehensive prenatal care helps identify and manage health issues early, ensuring better outcomes for both the mother and child. Without equitable access to these services, the risk of pregnancy-related complications and deaths increases significantly.
| Key Point | Details |
|---|---|
| Maternal Mortality Rate in the U.S. | The U.S. has the highest maternal mortality rate among high-income countries, with a rate of 32.6 deaths per 100,000 live births in 2022. |
| Preventable Deaths | Over 80% of pregnancy-related deaths in the U.S. are preventable. |
| Disparities in Death Rates | Significant disparities exist across racial and ethnic groups, with American Indian and Alaska Native women facing the highest rates. |
| Impact of COVID-19 | The sharpest increase in maternal mortality rates correlated with the COVID-19 pandemic onset in 2020. |
| Leading Cause of Maternal Deaths | Cardiovascular disease is currently the leading cause of pregnancy-related deaths in the U.S. |
| Late Maternal Deaths | Nearly one-third of maternal deaths occur between 42 days and one year after pregnancy, yet are often not included in maternal mortality statistics. |
Summary
Maternal mortality is a pressing public health issue in the United States, as it currently holds the highest rate among high-income nations. Despite the potential for prevention, many pregnancy-related deaths are still occurring, with significant disparities among different racial and ethnic groups. It is crucial for policymakers, healthcare providers, and communities to address these disparities, enhance prenatal and postpartum care, and invest in robust public health infrastructure to turn the tide on this alarming trend. To improve maternal health outcomes, a comprehensive approach to care and support during and after pregnancy must be adopted, focusing on accessibility and equity.